Frequently Asked Questions
-
Can you explain the difference between the types of VA claims?
There are numerous types of claims that apply to disability compensation. They can be based on disabilities that existed when entering military service, but were made worse, disabilities that occurred during service, or disabilities that arose after you left military service. Additionally, there are claims that are filed for special circumstances.
Pre-Discharge Claims
Service members that are within 180 days of separation or retirement from active duty or full time National Guard duty may file claims for disability compensation. Learn more about pre-discharge claims.Claims Based on Pre-Service Disabilities
Individuals may enter military service with a known disability. Should this disability become worse due to military service, VA may be able to pay compensation. This is known as aggravation; however, compensation can only be paid for the level of aggravation. For example, at entry into military service, an individual has a disabling condition that could be considered 10% disabling. In order for this condition to be considered aggravated, it would have to have worsened due to military service to at least 20%.Claims Based on In-Service Disabilities
These claims are based on disabilities that are a result of an injury or disease that occurred in active service, and in the line of duty. Injuries or diseases as a result of the Veteran’s own willful misconduct or abuse of alcohol or drugs are excluded.Claims Based on Post-Service Disabilities
Claims for post-service disabilities would include claims for disabilities that are a result of disabilities considered to be service-related, even though the disability arose after service. There are various classifications of presumptive disabilities which can be based on location or circumstances of service or just by military service itself. Learn more about post service claims.Claims Based on Special Circumstances
Claims regarding compensation are not always based on an in-service event. In other words, after a disability has been determined to be service connected, there may be other types of claims a Veteran or surviving spouse may wish to file. This might include a claim for a temporary 100% rating due to surgery for a service-connected disability, or additional compensation based on being in need of regular aid and attendance. Learn more about special claims. -
Can you explain the difference between the types of VA compensation?
VA disability compensation provides monthly benefits to Veterans in recognition of the effects of disabilities, diseases, or injuries incurred or aggravated during active military service. The program also provides monthly payments to surviving spouses, dependent children, and dependent parents in recognition of the economic loss caused by a Veteran’s death during military service or, after discharge from military service, as a result of a service-connected disability.
A summary of VA’s disability compensation programs is below:
Disability Compensation
A tax-free monetary benefit paid to Veterans with disabilities that are the result of a disease or injury incurred or aggravated during active military service. The benefit amount is graduated according to the degree of the Veteran’s disability on a scale from 10 percent to 100 percent (in increments of 10 percent). Compensation may also be paid for disabilities that are considered related or secondary to disabilities occurring in service and for disabilities presumed to be related to circumstances of military service, even though they may arise after service. Generally, the degrees of disability specified are also designed to compensate for considerable loss of working time from exacerbations or illnesses. Learn more about Disability Compensation.Dependency and Indemnity Compensation (DIC)
DIC is a tax-free monetary benefit generally payable to a surviving spouse, child, or parent of Service members who died while on active duty, active duty for training, or inactive duty training, or to survivors of Veterans who died from their service-connected disabilities. Parents DIC is an income-based benefit for parents who were financially dependent on of a Service member or Veteran who died from a service-related cause. Learn more about DIC and Parents DIC.Special Monthly Compensation (SMC)
SMC is an additional tax-free benefit that can be paid to Veterans, their spouses, surviving spouses and parents. For Veterans, Special Monthly Compensation is a higher rate of compensation paid due to special circumstances such as the need of aid and attendance by another person or by specific disability, such as loss of use of one hand or leg. For spouses and surviving spouses, this benefit is commonly referred to as aid and attendance and is paid based on the need of aid and attendance by another person. Learn more about Special Monthly Compensation.Claims Based on Special Circumstances
Veterans may be eligible for other types of disability compensation once a disability has been determined to be service connected. Special VA disability compensation programs include: individual unemployability, automobile allowance, clothing allowance, prestabilization, hospitalization, convalescence, dental, and birth defects. Learn more about special claims. -
How does VA classify claims?
Original Claim
An original claim is the first claim you file for compensation from VA. This can be filed by a Servicemember, Veteran or survivors of deceased Veterans.Reopened Claim
A reopened claim is a claim filed for a benefit that could not be granted and the decision has become final, meaning that it is over one year old and has not been appealed. VA cannot reopen these claims unless new and material evidence is received. New evidence is evidence that the VA has never before considered in connection with the specific benefit claimed. Material evidence is evidence that is relevant to and has a direct bearing on the issue at hand.Example 1
A Veteran was treated several times during service for pain in the right elbow. He filed a claim for service connection in 1989, but his claim could not be granted because no orthopedic abnormalities were found on VA examination. Two years later, his private physician x-rayed the elbow and noted arthritic changes in the joint. The Veteran submitted the new evidence to VA. Because it suggested a residual of his in-service elbow problems did exist, VA reopened his claim.Example 2
A Veteran was discharged from service in 1977. He filed an original claim for service connection for pes planus (flat foot) 20 years later. VA was unable to grant his claim because pes planus was never noted in the Veteran’s service treatment records. In 2001, he attempted to reopen his claim by submitting a statement from his private physician confirming the diagnosis of pes planus. VA was unable to reopen the claim because, while the evidence was “new,” it was not “material,” in that it failed to demonstrate the Veteran was diagnosed with pes planus during service.New Claim
A new claim is a claim for a benefit that may or may not have been filed before. Generally, the decision made on the claim is based entirely on new evidence. These may include claims for:
• An increased disability evaluation
• Special monthly compensation
• Individual unemployabilityA new claim differs from a reopened claim in that a decision on the claim is totally independent of any evidence submitted in connection with an earlier claim.
Secondary Claim
These are claims for disabilities that developed as a result of or were worsened by another service-connected condition. In other words, it is recognized that a service-connected disability may cause a second disability. This second disability may not otherwise be considered service-connected.Example 1
A Veteran has a service-connected knee injury that causes him to walk with a limp. He subsequently develops arthritis in his hip. Although the arthritic condition was not incurred during or aggravated by service, service-connection may still be established if the arthritis is a result of his knee condition.Example 2
A Veteran was in the Army for twenty years. During her military service, she was diagnosed with hypertension. After her discharge, service-connection was established for hypertension. She was subsequently diagnosed with a heart condition. Service-connection for her heart condition may be established as secondary to the hypertension. -
Can you explain the VA claims process?
There are eight distinct steps that most claims for disability compensation follow. These phases may vary in time depending on the complexity of the claim, the amount of evidence that must be gathered to support the claims, and the type of evidence. You are strongly encouraged to submit as much evidence as possible with your claim to help minimize processing time. The eight steps of claims processing are as follows:
Step 1. Claim Received
Your claim has been received by the VA. If you applied online with VONAPP Direct Connect, you should see receipt in your list of Open Claims within one hour. If you applied through the U.S. mail, please allow mailing time plus one week for us to process and record receipt of your claim.Step 2. Under Review
Your claim has been assigned to a Veterans Service Representative and is being reviewed to determine if additional evidence is needed. If we do not need any additional information, your claim will move directly to the Preparation for Decision phase.Step 3. Gathering of Evidence
The Veterans Service Representative will request evidence from the required sources. Requests for evidence may be made of you, a medical professional, a government agency, or another authority. It is common for claims to return to this phase, should additional evidence be required.Step 4. Review of Evidence
We have received all needed evidence. If, upon review, it is determined that more evidence is required, the claim will be sent back to the Gathering of Evidence phase.Step 5. Preparation for Decision
The Veterans Service Representative has recommended a decision, and is preparing required documents detailing that decision. If more evidence is required, the claim will be sent back in the process for more information or evidence.Step 6. Pending Decision Approval
The recommended decision is reviewed, and a final award approval is made. If it is determined that more evidence or information is required, the claim will be sent back in the process for more information or evidence.Step7. Preparation for Notification
Your entire claim decision packet is prepared for mailing.Step 8. Complete
The VA has sent a decision packet to you by U.S. mail. The packet includes details of the decision or award. Please allow standard mailing time for your packet to arrive before contacting a VA call center. -
How long will the claim process take?
The length of time it takes to complete a claim depends on several factors, such as the type of claim filed, complexity of your disability(ies), the number of disabilities you claim, and the availability of evidence needed to decide your claim.
You can track the status of your claim by registering for eBenefits at www.ebenefits.va.gov. You can also visit VA’s ASPIRE web site. Here you can find the average processing days for the regional office that is working on your claim. To find the average processing days for your state:
• Find your state on the map, place your cursor within the state and click
• This will open the Veterans Benefits Administration Aspire • Benefits site. Click “Enter”
• You should see a split table. On the left table click on “Compensation”
• This will expand the table. Approximately five rows down is “Rating Claims Processing Time”
• Follow that row to the right until you locate the cell located within the column of your regional office.The number you see is the average processing days to complete a claim that requires a disability rating. The average is based on completed claims since October 1 in a given fiscal year.
-
Why does the claim process take so long?
In Louisiana, compensation and pension claims take approximately 4-6 months. However, some of LDVA’s Veterans Assistance Counselors have seen a Pension Claim come back approved in 3 weeks. They’ve also seen compensation claims that are still pending 8 months after being submitted. Individual claim times vary depending on how many disabilities were claimed (Comp claim) or how much research has to be done (Pension claim). Individual claim processing times are affected by a myriad of factors, including Federal VA backlogs so there is no way of being able to predict the exact timeline.
-
What evidence requirements do I need to file a claim?
You must submit all relevant evidence in your possession and/or provide information sufficient to enable VA to obtain all relevant evidence not in your possession. This includes the following as part of your application:
• Discharge or separation papers (DD214 or equivalent)
• Service Treatment Records if they are in your possession (see the Veterans Records Destroyed in 1973 Fire if you suspect your records may have been involved in the 1973 NPRC fire)
• Medical evidence (doctor & hospital reports)Fully Developed Claim
VA established the Fully Developed Claim Program to expeditiously process claims certified by the claimant or his/her representative as meeting the Fully Developed Claim criteria. In order for you to participate in the Fully Developed Claim Program, you must obtain the relevant service treatment and personnel records and provide them to VA.
If VA decides your claim before one year from the date it is received, you will still have the remainder of the one-year period to submit additional information or evidence necessary to support your claim. For this program, VA will only obtain service treatment records and Federal treatment records when you identify them. More information about this program is available on the Fully Developed Claims page.Standard Claim
As a standard claim, VA is responsible for getting relevant records from any Federal agency that you adequately identify and authorize VA to obtain.
VA will make every reasonable effort to obtain relevant records not held by a Federal agency that you adequately identify and authorize VA to obtain. These may include privately held evidence and information you tell us about (such as records from a private doctor or hospital) and/or records from State or local governments or current or former employers.VA will provide a medical examination for you, or get a medical opinion, if determined it is necessary to make a claims decision.
Veterans Claims Assistance Act (VCAA)
In November 2000, Congress passed the Veterans Claims Assistance Act (VCAA) to define what VA’s responsibilities are in assisting claimants in obtaining evidence to support a claim and also to define the responsibilities of the claimant. VCAA responsibilities are as follows:
• Obtaining relevant records from any Federal agency. This may include records from the military, VA Medical Centers (including private facilities where VA authorized treatment), or the Social Security Administration.
• Providing a medical examination, or obtaining a medical opinion, if determined it is necessary to decide the claim.
A Claimant’s Responsibilities include:
• Obtaining relevant records not held by a Federal agency. This may include records from State or local governments, private doctors and hospitals, or current or former employers. VA may assist in obtaining these records.
• Providing enough information to VA so that records may be requested.Example
A Veteran has filed a claim for disability compensation and, on the application, indicated treatment from a private doctor and an award of Social Security disability. In this case, VA would be responsible in obtaining the Social Security records and would assist in obtaining the private physician records, but ultimate responsibility in obtaining the private records would be with the Veteran. -
What is the difference between 100% Individual Unemployability and 100% Total and Permanent?
100% Individual Unemployability is usually a Veteran whose disability rating falls at 70, 80, 0r 90%, but because their Service Connected issues they cannot work. This being the case, they are paid at the 100% rate, but retain their 70, 80, or 90% rating.
100% Rating, if it is not Total and Permanent, means that the Veteran has a disability that the VA feels may improve, and is reserving the right to re-rate that issue at a later date. This rating is usually in place for 3-5 years.
100% Total and Permanent is given to the Veteran when there is not a disability that needs to be re-rated. There are a few more benefits that kick in at this stage, including ChampVA for dependents, and Chapter 35 Dependents Educational Assistance.
-
What state benefits am I entitled to as a veteran in Louisiana?
If you are a Louisiana resident and an honorably discharged veteran verified by a DD214, you are entitled to:
-be interred in any state veterans cemetery at no cost to the veteran to include your spouse which will include a small fee
-receive a Louisiana Honor Medal in appreciation for your military service.
-have the word “VETERAN” placed under your picture on your driver’s license all renewal or replacement fees still applyIf you are 50% or greater service connected disabled you are entitled to:
-all of the above plus:
-free hunting and fishing license for the state of Louisiana, to include WMA permit and deer and turkey tags
-a disabled veteran (DV) license plate or a military honor (MH) license plate with a onetime processing fee
-free admission pass to all state parks and world heritage sites within the state of Louisiana
-free drivers license for the state of LouisianaIf you are 70% or greater service connected disabled you are entitled to:
-all of the above plus you are authorized to utilize the state veterans homes at no cost to the veteran.If you are 90% or greater service connected disabled you are entitled to the following:
-all of the above plus education assistance for your dependents and/or spouse in the state of LouisianaIf you are 100% service connected or 100% with individual unemployability (IU) you are entitled to the following:
-all of the above plus a tax break on your parish property taxes -
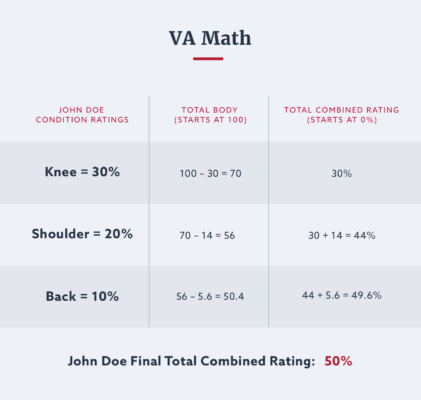
If I have multiple disabilities i.e., knee 30%; shoulder at 20% and back at 10%. These add up to 60% but the VA has only allowed me 50%. I don’t understand how they do this?
Hopefully, this graphic will offer a better explanation: